Back in 2012, I shared a chart showing that workplace deaths declined substantially after the creation of the Occupational Safety and Health Administration.
But I then shared a second chart showing 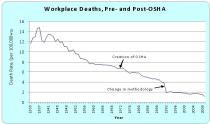 that workplace deaths declined just as much before OSHA was created.
that workplace deaths declined just as much before OSHA was created.
The moral of my story was quite simple. Deaths primarily fell because America become much more prosperous. And there’s a lot of evidence that wealthier is healthier.
Today, let’s look at a similar example.
A study published by the National Bureau of Economic Research looks at the impact of public health measures in the early 1900s. They start by sharing some good news.
Since the mid-19th century, mortality rates in the Western world have plummeted and life expectancy has risen dramatically. Sometimes referred to
as the mortality transition, this development is widely recognized as one of the most significant in the history of human welfare (Fogel 2004). Two features characterize the mortality transition. First, it was driven by reductions in infectious diseases and diseases of infancy and childhood (Omran 2005; Costa 2015). Second, it was concentrated in urban areas.
Do government policies deserve the credit?
There’s some evidence for that hypothesis.
…recent reviews of the literature emphasize the role of public health efforts, especially those aimed at purifying the water supply. For instance, Cutler et al. (2006) argue that public health efforts drove the dramatic reductions in food- and water-borne diseases at the turn of the 20th century. Similarly, Costa (2015) argues that clean-water technologies such as filtration and chlorination were “the biggest contributor[s] to the decline in infant mortality”
To be sure, there were huge public projects in the first several decades of last century. Here’s the data on sewage treatment facilities.
And here’s some data on milk purification efforts.
And the study has data on other aspects of public health as well.
The key question is whether all these efforts were successful. The three authors decided to investigate.
Using data on 25 major American cities for the years 1900-1940, the current study revisits the causes of the urban mortality decline at the turn of the 20th century. Specifically, we conduct a statistical horse race that attempts to distinguish the effects of ambitious, often extraordinarily expensive (Costa 2015, p. 554), public health interventions aimed at controlling mortality from food-and-water-borne diseases. Following previous researchers (Troesken 2004; Cutler and Miller 2005; Beach et al. 2016; Knutsson 2018), we explore the extent to which filtering and chlorinating drinking water contributed to the decline in typhoid mortality observed during the period under study and, more generally, to the observed declines in total and infant mortality. In addition, we explore the effects several other municipal-level efforts that were, at the time, viewed as critical in the fight against typhoid and other food- and water-borne diseases (Meckel 1990; Levitt et al. 2007; Melosi 2008) but have not received nearly as much attention from modern-day researchers. These interventions include: the treatment of sewage before its discharge into lakes, rivers and streams; projects designed to deliver clean water from further afield such as aqueducts and water cribs; requirements that milk sold within city limits meet strict bacteriological standards; and requirements that milk come from tuberculin-tested cows. Because the urban mortality transition was characterized by substantial reductions in infant and childhood mortality (Omran 2005) and because exclusive breastfeeding was not the norm during the period under study (Wolf 2001, 2003), improvements in milk quality seem a particularly promising avenue to explore.
But here’s the surprising result.
They did not find much evidence that public health efforts made a difference.
…our results suggest that the building of a water filtration plant cut the typhoid mortality rate by nearly 40 percent. More generally, however, our results are not consistent with the argument that public health interventions drove the extraordinary reductions in infant and total mortality observed between 1900 and 1940. Specifically, we find that efforts to purify milk had no appreciable effect on infant mortality and no effect on mortality from non-pulmonary tuberculosis (TB), which was often transmitted through infected milk. Likewise, neither chlorinating the water supply nor constructing sewage treatment plants appears to have been effective. …Our results point to other factors such as better living conditions and improved nutrition as being responsible for the sharp decline in urban mortality at the turn of the 20th century.
Here’s the chart showing that infant mortality consistently declined, largely independent of public health efforts.
I’m not suggesting, by the way, that public health spending is bad. Nor am I asserting that it’s a waste of money.
Notwithstanding some of the jokes that target libertarians, the goal isn’t to abolish every regulation or program governing safety and health. Maybe I’m a bad libertarian, but I’d pick a city with sewage treatment over one without.
But my main point is that I don’t need to make that choice. Nobody does.
The data strongly suggests that economic growth and rising levels of prosperity are the real drivers of improved health outcomes. Market-driven prosperity is what generates the wealth needed to improve public health, whether the actual delivery takes place via public or private action.




